All vaccines are thoroughly tested to ensure they are safe and work before they are licensed and used in the community. After being licensed vaccine safety continues to be monitored to ensure there are no extremely rare reactions that only occur when hundreds of thousands of doses have been given. This article explains common, uncommon and rare reactions to vaccines that have been identified through pre-licensing testing and ongoing safety monitoring.
Adverse events following immunisation
Anything undesirable occurring after a person receives a vaccine is called an Adverse Event Following Immunisation (AEFI) whether or not it is related to the immunisation. Some events, like getting a runny nose or cough, happen quite often during childhood and it is a coincidence that one starts just after immunisation rather than it being caused by the immunisation. Other events are known to be caused by immunisation.
Vaccine reactions reflect our body’s immune system responding to the immunisation. Not every person receiving a vaccine has a noticeable reaction. Some may have only one noticeable reaction and others may experience two or more.
Common, expected reactions
Common, expected vaccine reactions happen quite frequently. They may involve the whole body such as fever, feeling tired, sleepiness, being irritable, nausea, vomiting, diarrhoea or rash, or they may be where the vaccine was given such as soreness/pain, redness and/or swelling. These vaccine reactions may begin as early as six hours after immunisation. They are temporary, usually mild and go way without any treatment.
Uncommon, expected reactions
Some vaccine reactions are expected and happen somewhere between frequently and rarely. They are uncommon reactions and may include the whole body such as a very high fever (more than 39°C) or they may be where the vaccine was given such as severe pain or extensive swelling that covers the whole upper arm or leg where the vaccine was given. They are temporary and go away without any treatment.
Rare or very rare reactions
The very rare reaction that can occur after receiving any immunisation is a severe allergic response, called anaphylaxis, to an ingredient in the vaccine. The doctors and nurses giving immunisations are trained to manage anaphylaxis and have all the equipment needed. Up to three immunisations out of every one million given can cause anaphylaxis. There is a risk of anaphylaxis every time a person has an immunisation and this is why you and your child are asked to wait at the clinic for 20 minutes are receiving an immunisation.
Other rare or very rare but possible vaccine reactions depend on which immunisation has been given.
The table at the end of this page shows the possible vaccine reactions following each of the immunisation visits on the National Immunisation Schedule. Some common and uncommon vaccine reactions depend on the age of the child receiving the vaccine and how many doses they’ve already had. More detailed information about the individual vaccines is available on the Immunisation Advisory Centre website.
Managing vaccine reactions
Some of the ways to help your baby or child feel more comfortable after immunisation include:
- Give them lots of cuddles and fluids. If you are breastfeeding they may want lots of feeds.
- Do not rub or massage the injection site.
- If the injection site looks sore, red and/or swollen place a cool cloth, or a well wrapped ice pack, over the injection site.
- If they feel hot or have a fever undress them until they only have one layer of clothing, such as a singlet and nappy, until they’ve cooled down.
- Check that the room isn’t too hot or too cold.
- Consider using medication:
- If your baby or child is unsettled or miserable because of pain at the injection site or fever you can give them paracetamol or ibuprofen to help them feel more comfortable. It is very important to follow the dose instructions on the bottle because more than the recommended amount can be dangerous.
- Giving paracetamol or ibuprofen ‘just in case’ they are going to have pain or fever after immunisation is NOT recommended because it is possible that these medicines can affect their immune response to the vaccines.
If you have any concerns about how your baby or child is reacting to immunisation call your doctor or Healthline on their free phone number 0800 611 116 (24 hours a day, every day).
Vaccine reactions and the next immunisation visit
The only vaccine reaction that means a person must never have a particular vaccine again is a severe allergic reaction, called anaphylaxis.
It is safe for people who have had common and uncommon vaccine reactions to have the same vaccine again. It is really important that they have all the vaccine doses needed to protect them from the diseases covered by the vaccine.
If a person has had a rare or very rare vaccine reaction, other than anaphylaxis, it is important that a doctor with specialised medical knowledge about the reaction, and often a doctor with specialised immunisation knowledge, and the person or their parents discuss whether the risks from getting the disease or diseases covered by the vaccine are more serious than the risk of the rare reaction happening again. They can then decide whether to complete the number of vaccine doses needed for protection.
Useful links
The Immunisation Advisory Centre website.
The Ministry of Health immunisation webpage.
The Fight Flu website.
The World Health Organization immunisation webpage.
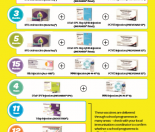
Immunisation visits and possible vaccine reactions
| Immunisation visit6 weeks, 3 months, 5 months | Possible vaccine reactions |
| Vaccine brand namesInfanrix®-hexa and
Synflorix®
Diseases these vaccines protect against Diphtheria Tetanus Whooping cough (pertussis) Polio Hepatitis B Haemophilus influenzae type b (Hib) Pneumococcal |
Common:
Uncommon:
Rare or very rare:
|
| Immunisation visit15 months | Possible vaccine reactions |
| Vaccine brand names Act-HIB™,
Synflorix® and M-M-R® II
Diseases these vaccines protect against Haemophilus influenzae type b (Hib) Pneumococcal Measles Mumps Rubella |
Common:
Uncommon:
Rare or very rare:
|
| Immunisation visit4 years | Possible vaccine reactions |
| Vaccine brandsInfanrix®-IPV and
M-M-R® II
Diseases these vaccines protect against Diphtheria Tetanus Whooping cough (pertussis) Polio Measles Mumps Rubella |
Common:
Uncommon:
Rare or very rare:
|
| Immunisation visit11 years | Possible vaccine reactions |
| Vaccine brandBoostrix®
Diseases this vaccine protects against Diphtheria Tetanus Whooping cough (pertussis) |
Common:
Uncommon:
Rare or very rare:
|
| Immunisation visit12 years (girls only) | Possible vaccine reactions |
| Vaccine brandGardasil®
Disease this vaccine protects against Human papillomavirus (HPV) |
Common:
Uncommon:
Rare or very rare:
|
To read more about immunisation, read our series of Kiwi Families articles:
Where to get immunised gives you information on how to obtain immunisation for your child.
The New Zealand Immunisation Schedule
Informed Choice discusses the advantages and disadvantages of immunisation.
Useful Immunisation Websites
http://www.health.govt.nz/our-work/preventative-health-wellness/immunisation/new-zealand-immunisation-schedule – Information on the current immunisation schedule
The National Immunisation Advisory Centre website